About 10 per cent of Canadians suffer from asthma, the most common chronic disease among children and one of the leading causes of hospitalization. Yet we don’t really know why asthma makes it so difficult to breathe, so current treatments only address its symptoms and are not a long-term solution or cure. To better understand asthma and other lung diseases and work toward more effective remedies, Carleton University Systems and Computer Engineering researcher Leila Mostaço-Guidolin is combining a pair of cutting-edge technologies.
Mostaço-Guidolin and her colleagues in the Carleton-led TEAM (Tissue Engineering & Applied Materials) Hub are using advanced microscopy imaging techniques and 3D bioprinting to develop functional models of the human airway.
These models, and the intricate process of creating them, will allow researchers to see the mechanisms of asthma and other respiratory conditions at a cellular and molecular levels and, ultimately, to test potential interventions.
From Tissue Sample to Accurate Model
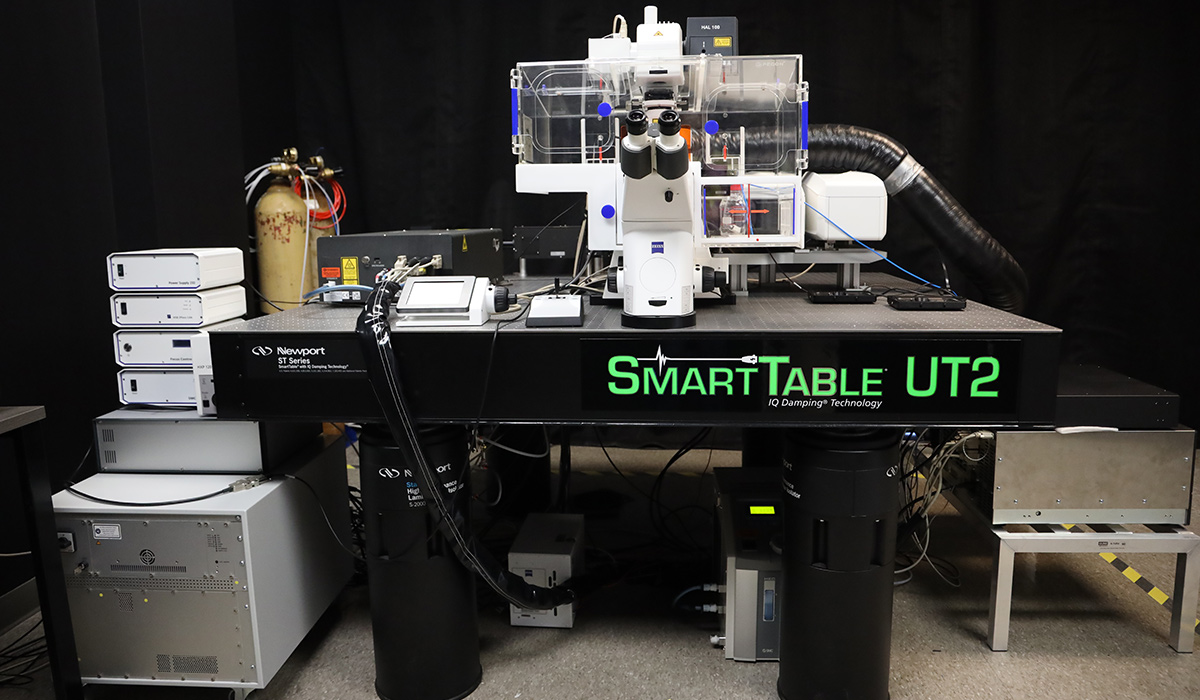
To replicate the human airway as accurately as possible, Mostaço-Guidolin starts with a lung tissue sample obtained from an organ donor or biopsy, which is looked at under an ultra high-resolution microscope.
The highly detailed images generated are analyzed to determine which cells are present, how they’re arranged and what the structure of the tissue looks like, and then a 3D bioprinter is used to “reverse engineer” this structure on an airway-like tube.
The printer uses a gelatin mix that contains collagen and proteins that occur naturally in human airways, giving the model real-world physical and chemical properties. And to further refine this process, the model itself can be microscopically imaged — “a feedback loop,” explains Mostaço-Guidolin, “so we can see how closely the structure we made resembles the real tissue and whether the cells are behaving as they should.”
Currently, Mostaço-Guidolin and her collaborators have a bioprinted hollow tube, with cells and proteins to give it structure, and are optimizing it so air can be perfused into the tube.
“We are trying to mimic the breathing process,” she says. “The ultimate goal is to have a structure similar to human airways and lung tissues — to have them surviving and interacting with one another in this artificial environment. Then we’ll be able to biochemically track what happens when the triggers of diseases like asthma make cells behave in a certain way.
“If you want to try to assess how a new drug might impact those cells,” she adds, “you can add this drug in the model, let the cells interact for a while, track changes within the tissue and see whether the drug is promising. This is an oversimplification of the whole process, but that’s one of the great applications of these in vitro models.”
Which Comes First: Fibrosis or Inflammation?
Not only is asthma a debilitating condition in need of attention, its basic mechanisms are similar to those of a range of diseases involving organs other than the lungs.
People with asthma have a hard time breathing because scar tissue narrows their airways. Scar tissue is related to the excess accumulation of collagen, which leads to what is called fibrosis. Fibrosis is related to inflammation, and according to Mostaço-Guidolin, trying to figure out whether inflammation triggers more fibrosis or vice vera is a chicken-and-egg situation.
“Bioprinted 3D models could be deployed to better understand the role of fibrosis in various cancers, cardiovascular diseases and other conditions,” she says. “The same mechanism affects different tissues and different organs throughout the body and we don’t know why this happens.
“To develop medicines, we need to know how we can interrupt this pathological behavior. Do we focus on the inflammation side of things, for example, or do we focus on repairing the scar tissue production?”

One of the benefits of the TEAM Hub approach it that the group brings together a cross-section of areas: researchers in biology, physics, health science and engineering are collaborating closely.
“Science has shifted a lot in the past few years,” says Mostaço-Guidolin.
“High-resolution imaging is creating new avenues for people working at the intersection of engineering, biochemistry and pharmacology domains. Now that we can connect with so many people and have access to so much information, we can tackle so many problems in a more targeted and meaningful way.”