Depression is one of the most significant challenges of our time, with over 280 million people suffering worldwide.
Despite the demand, antidepressants only have a 60 percent effectiveness rate, and it can take months on daily medication for patients to begin feeling better – a difficult wait for those already struggling with low mood or suicidal thoughts.
Carleton University neuroscientist Argel Aguilar-Valles is part of an international push to explore the therapeutic potential of a provocative subcategory of drugs: psychedelics.
“Psychedelics appear to reverse some of the damage that chronic stress causes, which enables the brain to be more resilient and better respond to the challenges we face in our lives,” says Aguilar-Valles.

In a recent study conducted in collaboration with the University of California at San Diego and the Medical College of Wisconsin, Aguilar-Valles found that 2-Bromo-LSD, a non-hallucinogenic derivative of lysergic acid diethylamide (LSD) developed by Vancouver-based pharmaceutical company BetterLife Pharma, could be a game-changing treatment option for depression and anxiety.
“The most widely prescribed type of antidepressant medication right now are selective serotonin reuptake inhibitors, or SSRIs, but it can be a trial-and-error process to see whether they work on a particular person,” says the Carleton researcher, noting that SSRIs can also cause unpleasant side effects like insomnia, stomach troubles and loss of sex drive.
“It’s virtually impossible to know who will be resistant, so people often spend years taking pills with minimal to no improvement.”
In contrast, early findings suggest that 2-Bromo-LSD could have fast-acting, long-term effects when it comes to treating mood disorders.
How Psychedelics Could Help Repair the Brain
The exact biological causes of depression remain unclear, but scientists do know that chronic stress can cause significant damage to the brain’s neurons, dulling our responses and reducing cognitive function.
“Neurons look a bit like trees,” Aguilar-Valles explains. “A depressed brain atrophied by chronic stress looks like a tree during winter, while a non-depressed brain is a healthy summer tree.”
He and other researchers found that psychedelics, a category drug which includes LSD and psilocybin (i.e. “magic mushrooms”), can help the brain repair some of that atrophy and “regrow its leaves.”
Unlike SSRIs, which trigger serotonin surges in our brain’s receptors, psychedelics are unique in that they bind directly to the receptors themselves. This causes profound changes in consciousness and encourages neuroplasticity – the ability of the brain’s neural network to rewire itself.
“Psychedelics are fascinating substances. They target and affect many different receptors in the brain in ways we don’t fully understand yet,” says Aguilar-Valles.
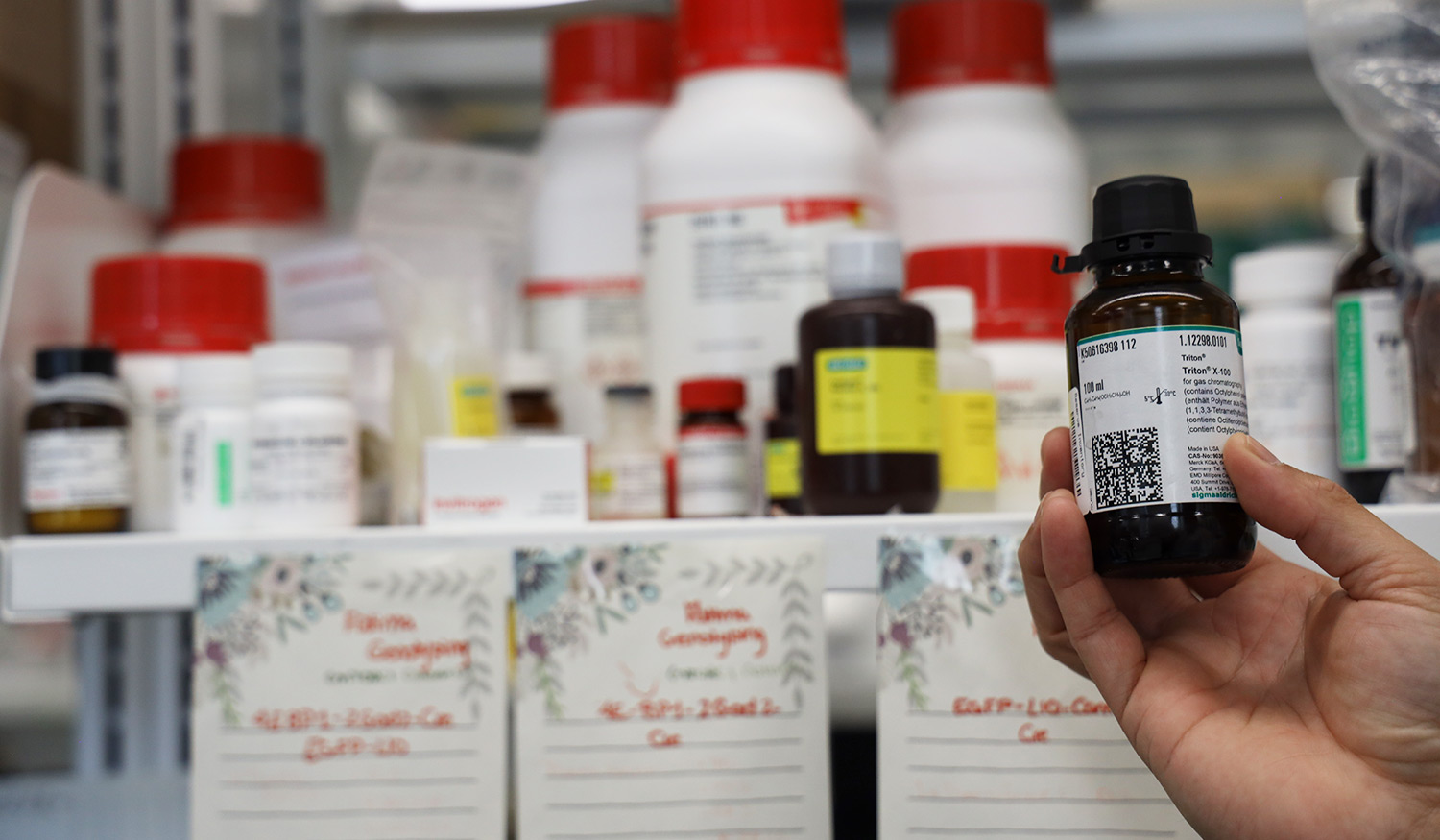
In 2021, while conducting research into using ketamine to treat major depression, Aguilar-Valles was contacted by BetterLife Pharma to test out the potential of 2-Bromo-LSD.
Synthesized in 1940 by Swiss chemist Albert Hofmann at the same time as regular LSD, the drug initially drew less attention compared to its flashier, hallucination-inducing sibling.
Today, the lack of “trip” is a major selling point for researchers as they explore whether 2-Bromo-LSD could work as an antidepressant, harnessing the power of its unique neurological profile without the inconveniences of sensory impairment.
A Renewed Research Path
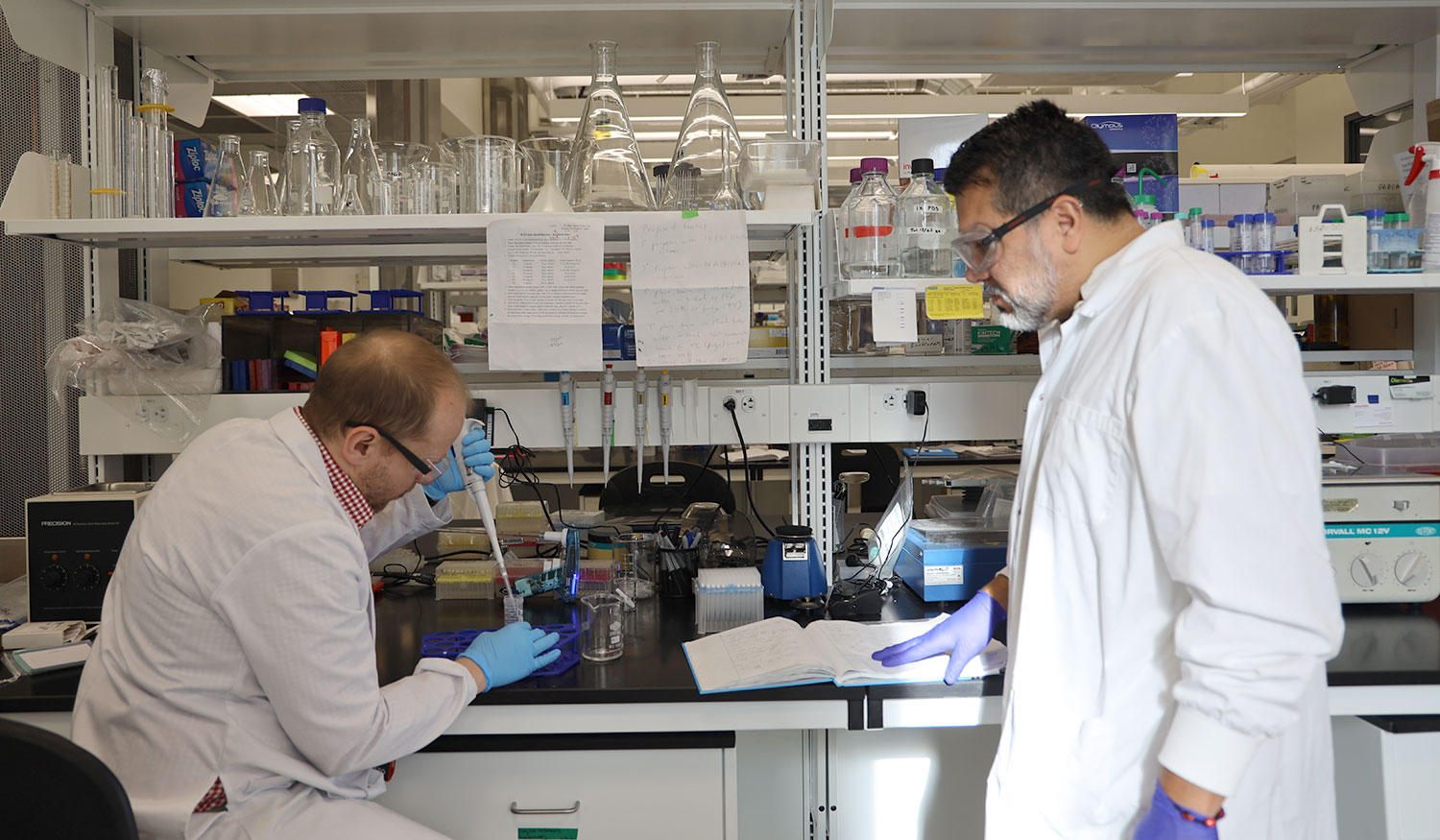
Initial findings from Aguilar-Valles’s lab in Carleton’s Department of Neuroscience suggest that the effects of 2-Bromo-LSD on the brain are immediate and impressively long-lasting. Instead of daily medication, a patient might only need a single dose every few months.
The drug is also showing potential as a treatment option for substance abuse disorders.
“LSD hits lots of different receptors, including dopamine receptors and the dopaminergic system itself,” explains Vern Lewis, a Carleton post-doctoral fellow working on the project. “Dopamine triggers feelings of reward and pleasure, so if this drug is hitting that system, it could be very useful at treating addiction.”
Notably, psychedelics themselves are not, at a chemical level, addictive substances.
“You’re not going to experience withdrawal or form a dependence on psychedelics. It’s like riding a motorcycle – you might really enjoy the experience, but you’re not going to suffer from withdrawal if you can’t go out for a ride,” says Lewis.
Labeling all recreationally used drugs as addictive and harmful is, in part, why research on psychedelics has remained stalled for decades.
“Decisions were made based on stigma and political opinions instead of science,” says Aguilar-Valles. “Canada used to be one of the leading countries for psychedelic research in the 70s, and there were clinical trials back then showing great promise for treating alcohol and tobacco use disorders. Then psychedelics were banned, access was restricted, and the research died down.”
Today, as scientists pick up where they left off and exploratory studies into psychedelics resume, Carleton’s Aguilar-Valles is advocating for cautious optimism.
“There’s a desperate need for help when it comes to depression, but we can’t rush the scientific process,” he reflects.
“It’s important to remember that more research and education is needed around what these drugs do and how they might one day be used for clinical purposes.”