Carleton University neuroscience researcher Michael Hildebrand has been exploring the causes of chronic pain for more than 15 years. A new project he’s helming — in collaboration with Eli Lilly and Company and The Ottawa Hospital, among others — could lead to a better understanding of what’s happening in the spinal cord to perpetuate this pain and how to develop drugs to treat it.

“This is a huge crisis because we’re dealing with debilitating pain as well as high health care costs and lost productivity,” says Hildebrand. “People may seem fine because they don’t always have outward signs, but it really impacts their ability to function.
“We really need to move the needle on pain research, and it’s an exciting time because we’re mobilizing to address this challenge.”
Although the brain processes pain signals and helps keep you alive by telling you something’s wrong, these sensory impulses are first organized in and travel through the spinal cord. For some people, pain ramps up when it shouldn’t — after an injury has healed, for instance.
Hildebrand believes we can treat pain more effectively by studying the spinal cord and chemically targeting areas where signals are relayed and amplified needlessly.
He and his students conduct experiments using spinal cord tissue from rats and human organ donors, the latter acquired through their unique partnership with neurosurgeon Dr. Eve Tsai at The Ottawa Hospital. They record electrical signals travelling between neurons and study the molecules that control the delivery of pain signals to the brain.
In a paper published earlier this year, their research showed, for the first time, that neurons in the spinal cords of men and women process pain signals differently — a discovery that could have implications for future drug development.
The Root Causes of Chronic Pain
Hildebrand and Annemarie Dedek, a Mitacs Industrial Postdoctoral Fellow at Carleton, are now working with scientists at Eli Lilly to further this research. They’re using cutting-edge high-definition multi-electrode arrays to enhance their understanding of the mechanisms of pain with the goal of developing new human tissue preclinical screening tests for pain therapies.
“Our focus is investigating the underlying physiology of the human spinal cord,” says Hildebrand.
“A key piece of that puzzle that’s missing is figuring out what’s happening to spinal cord circuitry when you activate these pain pathways or when you block them with treatments. This project will help us identify specific molecules and receptors that are potential drug targets.”
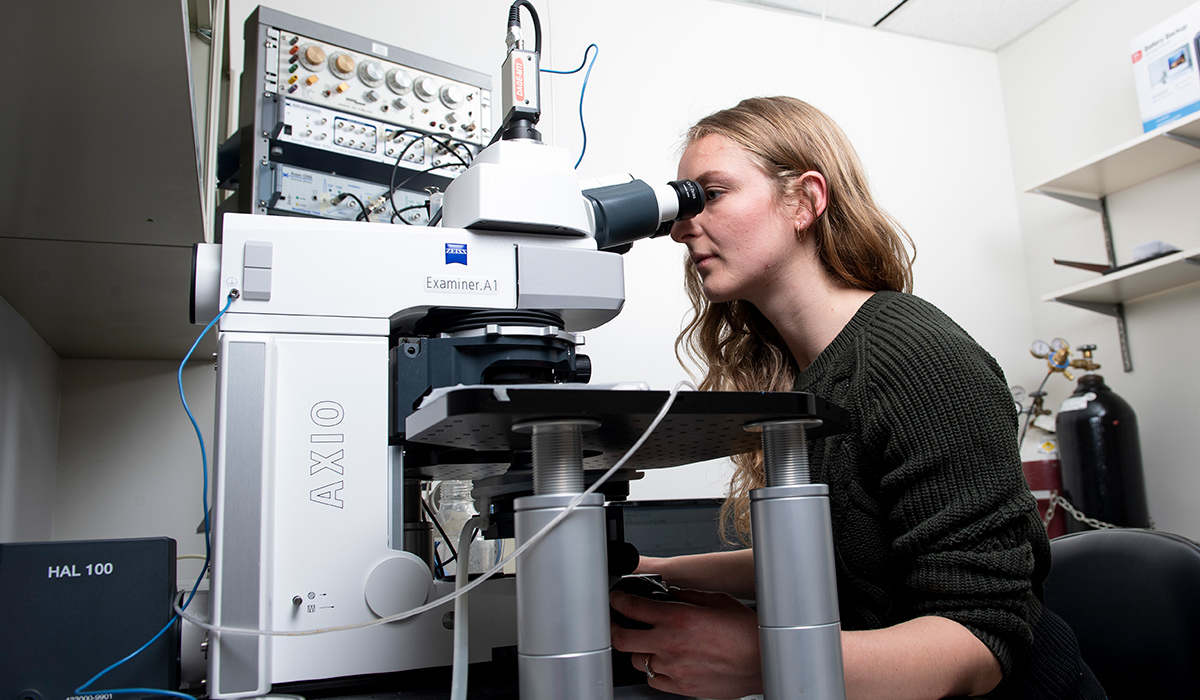
Using traditional electrical recording technology, researchers could only study what’s happening inside tissue samples one cell at a time. The multi-electrode arrays in Hildebrand’s lab at The Ottawa Hospital — tiny chips, about six millimetres by six millimetres, containing around 4,000 electrodes — can record the activity of hundreds of neurons at the same time.
“The cells in the spinal cord slices that we use are still communicating and firing,” explains Dedek, who handles the bulk of the hands-on work and relies on computer science specialists at Carleton to figure out how to store and manage the incredibly high volume of data.
“I can put a slice on a multi-electrode array and record activity from the entire circuit. That’s really powerful, because it lets us look at how cells are working in tandem and see circuit-level processes that could be involved in chronic pain.
“Once we understand this circuitry better,” she adds, “this technique could potentially be used to target some of the pathways that we’re studying to disrupt pain signals.”
The Chronic Pain Connection
Eli Lilly approached Hildebrand after seeing Dedek give a talk at a conference.
“Although the pharmaceutical industry has a greater number of resources than our academic colleagues, we don’t always have the ability to perform the exact experiments needed to test a hypothesis,” says Jeff Krajewski, an executive director of pain biology with the company.
“Advances in identifying novel biological mechanisms are typically developed by academic labs. Michael has been a major contributor to chronic pain research throughout his career. His interests aligned perfectly with ours: understanding the spinal mechanisms that underly chronic pain to aid the development of better therapies.”
“We want to move toward treatments, but I can’t do all of that in my lab,” says Hildebrand.
“That’s why this is such a natural partnership — Eli Lilly can use the same approaches we’re using to test how specific drugs affect spinal cord circuitry.”
“What keeps me going,” adds Dedek, “is the hope that we’ll have a future where chronic pain is better managed through safe, effective treatments.”